

Type 2, for example, generally involves mild immunodeficiencies, while type 1 causes severe combined immunodeficiency (SCID). The new codes under category D81 Combined immunodeficiencies were needed to differentiate between the types of adenosine deaminase deficiency. Codes under G43 Migraine and R11 Nausea and vomiting are revised to accommodate the new code.
TYPE II ATRIAL FLUTTER ICD 10 CODE
1, 2019, use new code R11.15 Cyclical vomiting syndrome unrelated to migraine to report this diagnosis. ICD-10-CM code R11.10 Vomiting, unspecified does not adequately represent the clinical significance of cyclical vomiting syndrome and the treatment of the disorder not related to migraines. The new codes under category Q66 Congenital deformities of feet are added to create consistency across all congenital foot deformities, which allows specification of side. New codes N63.15 Unspecified lump in the right breast, overlapping quadrants and N63.25 Unspecified lump in the left breast, overlapping quadrants allow for proper code assignment when an unspecified lump in the breast overlaps anatomic sites classifiable to different codes. Atrial FibrillationĬode changes under category I48 Atrial fibrillation and flutter were deemed necessary to maintain the term “chronic atrial fibrillation” in ICD-10-CM as it appears in the World Health Organization’s (WHO) ICD-10. Here are rationales for some of the new codes that go into effect Oct. 11-12, 2018, provide insight into the purpose of subsequent code changes, which can help you to use the updated code set more easily and efficiently.
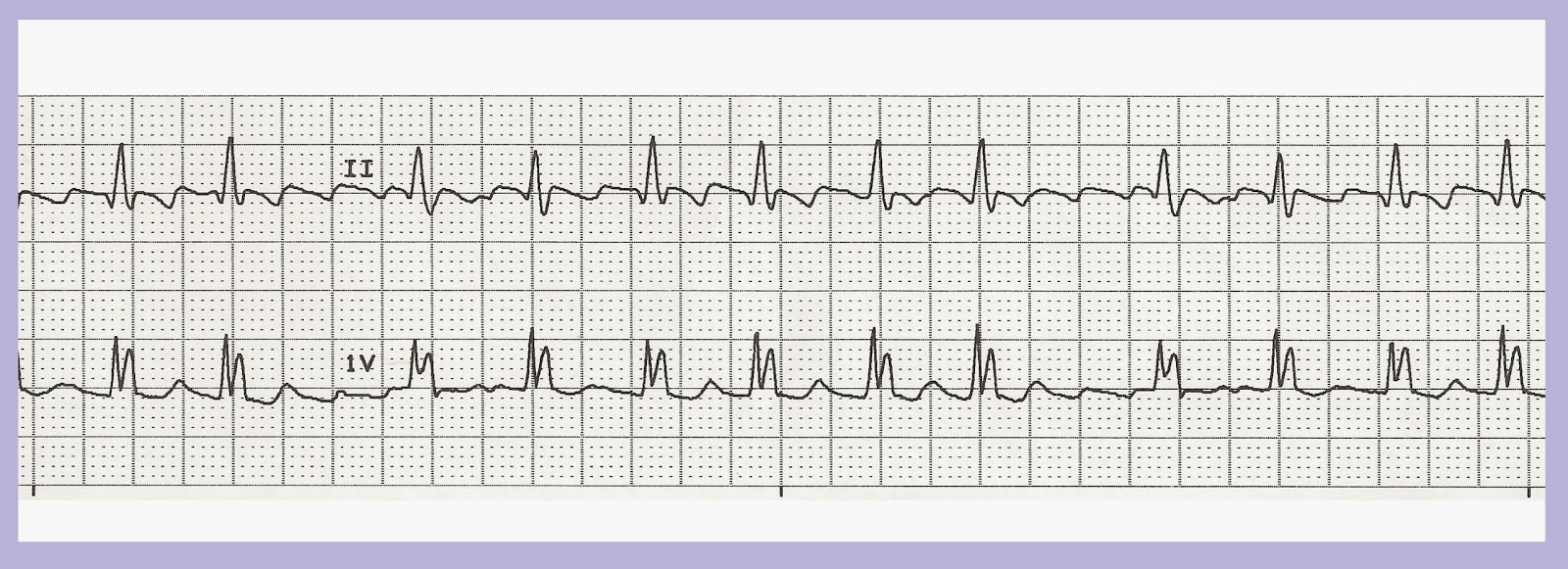
Many of the ICD-10-CM updates for 2020, presented at the ICD-10 Coordination and Maintenance Committee meeting on Sept. In the absence of additional arrhythmias, infants with AFL have an excellent prognosis once in sinus rhythm, with a low risk of recurrence, and chronic anti arrhythmic therapy is unlikely to be necessary.Rationales for ICD-10-CM updates are key to improved medical coding, data reporting, and physician reimbursement. Sotalol is said to be an effective agent in the treatment of AFL in the fetus as it has excellent transplacental passage. Recurrence of atrial flutter in neonates is rare and prophylactic medication is usually not required. The response to drug treatment is variable and unpredictable. This is most easily achieved by transoesophageal overdrive pacing or synchronised low energy DC cardioversion using around 0.5-1 J/kg. The first aim of treatment is the restoration of sinus rhythm. Antenatal diagnosisĪFL may be diagnosed prenatally by fetal echocardiogram which will show an atrial rate of over 400 per minute and most often 2:1 AV conduction to give a ventricular rate of over 200 per minute. Differential diagnosisĭifferential diagnosis includes multifocal atrial tachycardia (see this term) and other forms of supraventricular tachycardia. The echocardiogram may show impaired ventricular function after prolonged tachycardia. The diagnosis of AFL relies on surface electrocardiogram (ECG) which usually shows an atrial rate of around 440 beats/min, most often with 2:1 atrioventricular conduction (sometimes with variable AV conduction and an irregular ventricular rate of 125-280 beats/min), and saw tooth P waves in leads II, III, and aVF. The etiology of AFL is unknown but immaturity of the myocardium and the high pressure in the right atrium during the perinatal period may be factors that favor the appearance of atrial re-entry. Some patients are asymptomatic and tachycardia may be noted on routine examination and monitoring. AFL is sustained although conversion from atrial flutter to sinus rhythm may occur spontaneously (<24 hours). AFL manifests with tachycardia and congestive heart failure. Onset during the fetal period may be associated with hydrops fetalis and death.


Clinical descriptionĪFL has a neonatal onset and the majority (72%) of patients present with symptoms within the first 48 h of life. AFL is rare with an approximate incidence of around 1/50,000 live births in Europe.


 0 kommentar(er)
0 kommentar(er)
